In recent years, doctors around the world have placed strong emphasis on HPV vaccination, especially for young women. This recommendation is not based on trends or marketing it is grounded in decades of medical research and real-world evidence. Human Papillomavirus (HPV) is one of the most common viral infections globally, and while many HPV infections go away on their own, some types can silently lead to serious health problems later in life
Understanding why doctors encourage early vaccination can help young women and parents make informed, confident health decisions.
What Is HPV and Why Is It a Concern?
HPV is a group of more than 100 related viruses. Some types cause harmless skin warts, but others are considered “high-risk” because they can lead to cancers. The most well-known is cervical cancer, but HPV is also linked to cancers of the vagina, vulva, anus, throat, and mouth.
What makes HPV particularly concerning is that it often shows no symptoms. Many people don’t know they are infected, and the virus can stay in the body for years before causing cell changes that may eventually develop into cancer.
This silent nature of HPV is one of the main reasons doctors strongly promote vaccination early before exposure happens.
Why Vaccination Is Recommended at a Young Age
Doctors recommend HPV vaccination primarily for adolescents and young women because the vaccine works best before exposure to the virus. HPV is commonly transmitted through intimate skin-to-skin contact, and most people encounter it soon after becoming sexually active.
Vaccinating at a younger age allows the immune system to build strong, long-lasting protection well in advance. Studies consistently show that younger individuals produce a stronger immune response to the vaccine, making early vaccination both medically effective and strategically preventive.
The Real HPV Vaccine Benefits
The HPV vaccine benefits go far beyond avoiding a short-term infection. Doctors recommend the vaccine because it can:
• Protect against the HPV types responsible for most cervical cancer cases
• Reduce the risk of genital warts
• Lower the likelihood of abnormal Pap test results
• Decrease future need for invasive diagnostic procedures
• Offer long-term protection that can last decades.
By preventing high-risk HPV infections before they occur, vaccination dramatically reduces the chances of developing HPV-related cancers later in life.
HPV Vaccination and Cervical Cancer Prevention
Cervical cancer remains one of the most preventable yet still common cancers affecting women, particularly in countries where routine screening is limited. Persistent infection with high-risk HPV types is the leading cause of cervical cancer.
Doctors consider HPV vaccination one of the most powerful tools available today for cervical cancer prevention. When combined with regular gynecological check-ups and screening, vaccination creates a strong, layered defense against the disease.
Rather than waiting to detect abnormal cells years later, HPV vaccination focuses on stopping the problem at its source by preventing the infection that causes those changes in the first place.
Addressing Common Concerns
Some people worry about vaccine safety or long-term effects. Doctors recommend HPV vaccination because it has been extensively studied across millions of individuals worldwide. Ongoing global monitoring continues to confirm that the vaccine is safe, well-tolerated, and highly effective.
Typical side effects are mild and temporary, such as arm soreness, slight fever, or fatigue. Serious side effects are extremely rare. From a medical standpoint, the proven protection against cancer far outweighs these short-term discomforts.
Another important point doctors emphasize is that the HPV vaccine is preventive, not curative. It does not treat existing infections, which is why earlier vaccination offers the greatest benefit.
The Bigger Picture: Long-Term Women’s Health
Doctors are not only focused on preventing one infection they are looking at long-term quality of life. Cervical cancer treatments can involve surgery, radiation, and chemotherapy, which may affect fertility, pregnancy outcomes, and overall well-being.
HPV vaccination is recommended because it helps young women avoid facing these challenges later. It is a proactive step that supports reproductive health, emotional well-being, and future family planning.
When doctors advise vaccination, they are thinking years ahead toward adulthood, motherhood, and healthy aging.
Final Thoughts
HPV vaccination is not about fear it is about foresight. Doctors recommend it for young women because it offers safe, effective, and long-lasting protection against some of the most preventable cancers affecting women today.
By choosing vaccination early, young women give themselves a powerful advantage: protection before risk, prevention before treatment, and knowledge before uncertainty.
FAQs
1. At what age do doctors usually recommend the HPV vaccine?
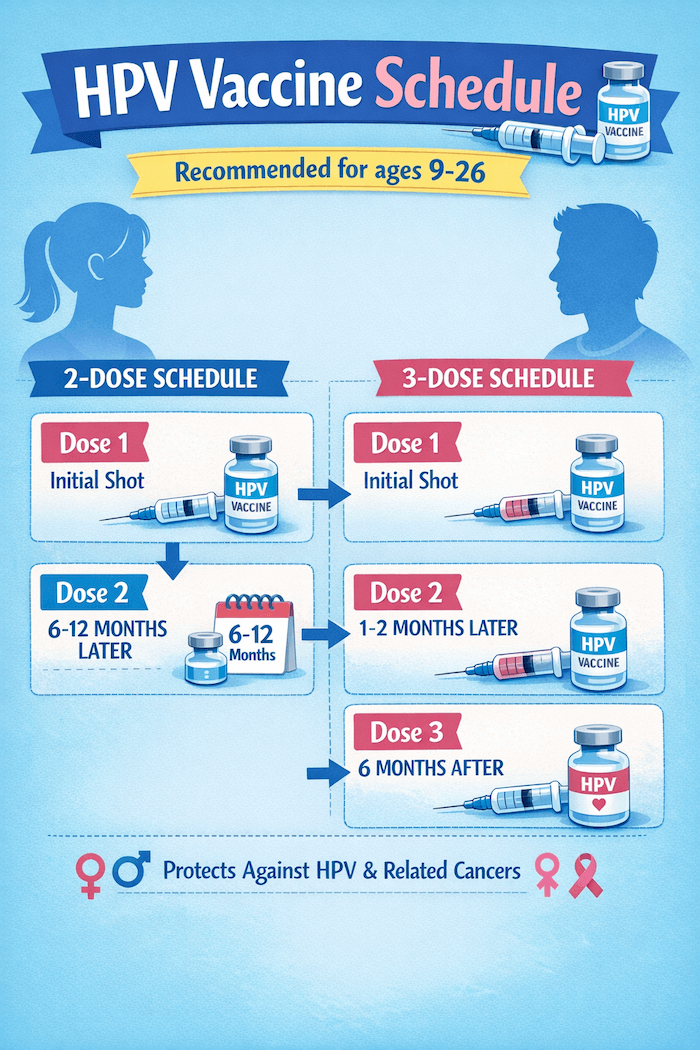
Doctors generally recommend vaccination in early adolescence, but young women who were not vaccinated earlier can still benefit. The exact age range may vary, but earlier vaccination provides the strongest preventive protection
2. Can someone still get the HPV vaccine if they are already sexually active?
Yes. Even if someone is sexually active, the vaccine can still protect against HPV types they have not yet encountered. Doctors often recommend it because exposure to one type does not mean exposure to all.
3. Does the HPV vaccine replace regular cervical screening?
No. Vaccination significantly reduces risk, but routine screening remains essential. Doctors recommend both vaccination and regular check-ups for complete protection.
4. Is the HPV vaccine only for cervical cancer?
No. While cervical cancer prevention is a major benefit, the vaccine also protects against other HPV-related cancers and genital warts, supporting overall long-term health.